TISSUE-ENGINEERED DISEASE MODELS
_edited.jpg)
For many years after its inception, the field of tissue engineering focused solely upon the generation of healthy tissues to repair or replace damaged organs. However, in recent years, the field has evolved to recognize the wide-ranging and near-term impacts that can be achieved through the application of tissue engineering techniques to model disease. My lab creates biomaterial platforms that mimic features of diseased tissue microenvironments, with a specific focus on how the composition and architecture of the extracellular matrix (ECM) influence disease progression. We merge the more traditional bottom-up construction of 3-D biomaterial scaffolds with a new top-down approach of ECM-editing ex vivo organ cultures, and apply these platforms to decipher the cues responsible for regulating disease pathogenesis. Our lab employs these disease-mimicking environments to study a wide range of tissues; you will find a few examples below, and more information on our publications page!
CELLULAR-SCALE SEX BIAS IN DISEASE PROGRESSION

Calcific aortic heart valve disease affects a LOT of people: over a quarter of all individuals over age 65! For many years, our lab has been interested in figuring out why heart valve disease happens. We use tissue engineering tools to create models of heart valves at different stages of disease and probe the molecular mechanisms of disease progression. Our hope is that this research will lead to the identification of a way to stop heart valve disease from progressing.
We were also the first lab to discover that valve cells from males behave differently than valve cells from females! Later, it was found that valve disease in men actually looks very different from valve disease in women. Thus, much of our current work focuses on discovering how and why the sexes diverge in their development of heart valve disease.
HEALING CHRONIC WOUNDS
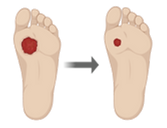
Over 6.5 million people in the U.S. have a chronic wound. These wounds are a cause of significant healthcare costs, as well as decreased quality of life and increased mortality. In collaboration with Prof. Pam Kreeger, our lab examines the cues that make cells migrate, in order to identify ways to stimulate better closure of wounds.
Through this work, we have uncovered novel information about the signals that drive cells to work in a collective manner to heal wounds, including information about why many other approaches to heal chronic wounds have failed. We are translating this information to create new approaches that stimulate wound closure.
.png)
.png)